42 yr old male
This is an online E-log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient centered online learning portfolio and your valuable comments on comment box is welcome.
I've been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and prognosis
A 42 year old male resident of Nerada,chityala mandal farmer by occupation came to the OPD with the chief complaints of
CHIEF COMPLAINTS:
Chest pain since 3 days
Vomitings since 3 days.
Loose motions since 3 days.
Shortness of breath since 2 days.
History of present illness :
patient was apparently asymptomatic 3 days back then he developed chest pain which was sudden in onset gradually progressive,crushing type of pain, non radiating in the lower part of the left chest, aggravated on lifting weights in agriculture fields and no relieving factors present.yesterday evening (4/10/23) chest pain suddenly increased and brought to the hospital.
H/o vomitings 3-4 episodes per day since 3 days, non bilious, non projectile,along with blood(hematemasis).
H/o loose motions since 3 days , 2-3 episodes per day associated with clots(melena)
H/o shortness of breath since 2 days, insidious in onset, gradually progressive,no aggrevating and reliving factors.
No H/o fever,chills and rigor,orthponea,pedal edema,abdominal distension,pain abdomen,PND.
History of past illness :
No similar compliants in the past
H/O 3 episodes of epilepsy in the past 3 yrs. last episode was 1 yr back for which he used medication for 6 months and then he stopped using medication.
No history of DM,HTN,TB,asthma,CAD,CVD.
No drug allergies presnt.
Family history : not significant.
Personal history :
Sleep : adequate
Diet : mixed
Appetite : normal
Bowel and bladder movements : irregular( loose motions 2-3 episodes).
H/o of alcohol consumption(brand name: officers choice,whisky) 180 ml every day since 15 years.
H/o khaini chewing since 14 years 1 pack per 2 days.
No H/o of smoking.
General examination :
Patient is conscious, coherent , cooperative well oriented to time, place and person.
Moderately built and nourished.
Pallor : absent
Icterus : absent
Cyanosis : absent
Pedal edema : absent
Generalised Lymphadenopathy : absent
Vitals :
BP : 110/70mmHg
Pulse : 74bpm
RR : 17 cpm
Temperature : afebrile
Spo2 : 99%
GRBS : 100 mg/dl
System examination :
Respiratory system examination :
Inspection :
Position of trachea central
No dropping of shoulders
No intercostal indrawing
No supraclavicular hallowness
Shape and symmetry of the chest normal.
No dilated veins.
No visible scars.
accessory muscles of respiration not prominent.
Palpation :
On three finger test : position of the trachea central.
Respiratory movements are normal.
Vocal framitus : Right. left
Supraclavicular area. N. N
Infraclavicular area. N. N Mammary area. N. N
Axillary area N. N
Infraxillary area N. N
Suprascapular area. N. N
Interscapular area. N. N
Infrascapular area. N. N
Normal and vibrations are equal in all areas.
Percussion :
Resonate note on Percussion in all intercostal spaces on both sides.
Tidal percussion: resonant note in the right 5 th intercostal space after deep inspiration.
Ascultation :
Vocal resonence :
Right left
Supraclavicular area. N. N
Infraclavicular area. N. N
Mammary area. N. N
Axillary area N. N
Infraxillary area N. N
Suprascapular area. N. N
Interscapular area. N. N
Infrascapular area. N. N
Normal vesicular breath sounds.
Bilateral air entry positive.
No crackles heard.
On abdominal examination:
Inspection:
Shape of abdomen is scaphoid
Flanks are free
Umblicus is in position, inverted
Skin over abdomen normal shiny, no scars, no sinuses, no nodules, no puncture marks.
No visible veins.
No engorged veins.
Movements of abdominal wall are normal, no visible gaatric peristalsis.
Palpation: All inspectory findings are confirmed by palpation.
No tenderness , No local raise of temperature.
Liver not palpable.
Spleen not palpable.
Percussion :
No ascitic fluid present.
Auscultation
Normal bowel sounds heard.
2. Bruit - no renal artery bruit heard.
no iliac artery bruit heard.
CVS Examination :
S1 and S2 sounds are heard, no trills and murmurs heard.
CNS Examination :
No focal neurological deficit present
Higher mental functions are intact.
H/o tremurs in hands present.
INVESTIGATIONS
Complete blood picture
Liver function test
Renal function test
Blood grouping
ECG
Chest x ray
X ray abdomen
MRI
ABG
Random blood sugar
Complete urine examination
2D echo
USG abdomen
Serology.
No pallor
No icterus
ECG :
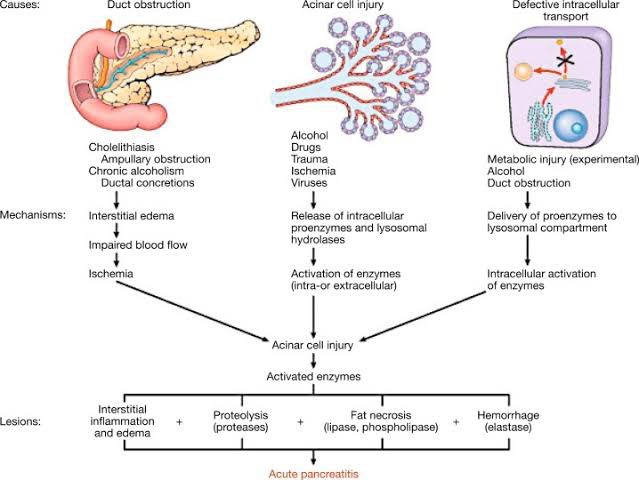
Provisional diagnosis : acute pancreatitis.
Treatment :
Pethidine, meperidine for pain relief.
Antibiotics: ceftazidime,cefoperazone,cefotaxime.
Nasgastric aspiration,nasal O2, TPN.
Calcium gluconate.
Redydration by normal saline 400 ml per hr ,ringer lactate solution.
Ranitidine
Electrolyte balance
Endotracheal intubation
Somatostatin.